


Circumcision is a procedure that has been practised for thousands of years, with various cultural, religious, and medical reasons behind its significance. For parents, the decision to circumcise their child can be a complex and emotional one, involving a blend of health considerations, cultural beliefs, and ethical reflections.
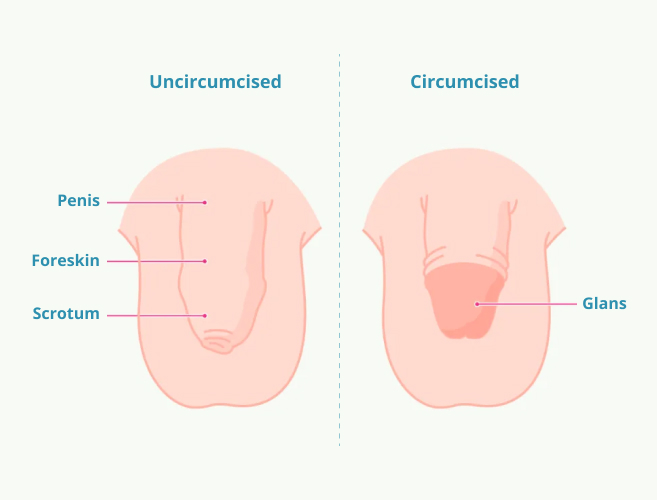
Circumcision is the surgical removal of the foreskin from the male genitalia, typically performed in infancy or early childhood, though some men choose to undergo circumcision later in life for medical or personal reasons. The procedure involves the removal of the skin that covers the head (glans) of the penis.
In some cultures and religions, circumcision is a rite of passage or a sign of belonging. In other cases, it is performed for its perceived health benefits, such as improved hygiene and reduced risk of certain infections. While circumcision is commonly associated with male infants, the practice is not limited to men only. Female circumcision, or female genital mutilation (FGM), is an unfortunate but real phenomenon that continues in some parts of the world.
The circumcision procedure is generally quick and relatively straightforward, but like any surgery, it carries some risks. Here’s what typically happens during the procedure:
Circumcision has certain health benefits that can influence parents to choose the procedure for their children. These benefits are backed by research and often mentioned by doctors.
Infants who are not circumcised have a higher risk of developing urinary tract infections, which can lead to kidney damage in severe cases. Circumcision reduces this risk by eliminating the environment where bacteria can accumulate under the foreskin.
Although penile cancer is rare, circumcision has been shown to lower the likelihood of developing this form of cancer. The removal of the foreskin reduces exposure to substances that may increase the risk of cancer.
Circumcised men are less likely to contract HIV, human papillomavirus (HPV), herpes, and syphilis. The removal of the foreskin decreases the number of sites where pathogens can enter the body during sexual activity, thus lowering the likelihood of transmission.
Circumcision makes it easier to maintain cleanliness in the genital area. The absence of the foreskin eliminates the need to manually retract the skin to clean the penis, which can reduce the buildup of smegma – a combination of dead skin cells, oils, and moisture.
A condition where the foreskin is too tight to be retracted over the glans is known as phimosis, and paraphimosis is when the retracted foreskin cannot be returned to its normal position. Both conditions can cause pain, infection, and other complications. Circumcision eliminates these risks.
Circumcision can reduce the transmission of human papillomavirus (HPV), which is linked to cervical cancer in women. By circumcising males, there may be a reduction in HPV transmission to female partners, lowering the risk of cervical cancer.
Although circumcision is generally considered safe, it is still a surgical procedure that carries some inherent risks. These may include bleeding, infection, or an adverse reaction to anaesthesia. Circumcision can be painful during the recovery period, especially for newborns and infants. Even though pain relief is typically provided, the healing process can cause discomfort and require several weeks to fully heal.
While the risk is low, infections can occur at the site of the incision. This can lead to complications such as redness, swelling, or discharge, requiring medical treatment. If the circumcision site isn’t properly cared for during the healing period, there could be a higher chance of developing infections like balanitis (inflammation of the glans) in the future.
Some men report a decrease in penile sensitivity after circumcision. The removal of the foreskin exposes the head of the penis, which may become less sensitive over time due to constant exposure to friction and touch. While many men experience no change in sexual function, some report a decrease in sexual pleasure or satisfaction. The foreskin contains specialised nerve endings, and its removal could affect sexual sensitivity.
Although infants may not have the memory of the procedure, there are concerns about the psychological impact of circumcision in early childhood. The emotional trauma and pain, even if temporary, could lead to distress or a sense of violation, though this is highly individual and may not apply to all. Older individuals, especially those who undergo circumcision later in life for medical reasons, may experience body image issues or feel self-conscious about their appearance or sexual function, particularly in a culture where circumcision is not the norm.
If the procedure is not performed correctly, there’s a risk of removing too much tissue, which could lead to scarring, changes in the appearance of the penis, or even functional problems, such as difficulty in retracting the remaining skin or pain during sexual intercourse. In rare cases, an inexperienced surgeon may cause disfigurement or damage to the penis, leading to permanent complications.
Over time, circumcision can lead to the formation of scar tissue, which might cause the penis to feel less flexible or mobile. This can sometimes lead to discomfort during sexual activity, and in rare cases, the scar tissue may cause erectile dysfunction or other issues. While circumcision can prevent phimosis (the inability to retract the foreskin), there are cases where the remaining foreskin can still become tight or cause other issues, leading to the need for further intervention.
Although circumcision is often covered by health insurance, it can be costly if done privately or for non-medical reasons. For families who choose circumcision for cultural or religious purposes, the cost may not be covered by insurance, creating a financial burden.
Whether circumcision is good or bad depends on various factors, including medical, cultural, ethical, and personal considerations. From a medical standpoint, circumcision can offer several health benefits, such as a reduced risk of urinary tract infections, sexually transmitted infections, and penile cancer. It also improves hygiene and can prevent conditions like phimosis. However, the procedure carries risks, including potential complications like infections, loss of sensitivity, and psychological impact, especially in infants who cannot consent.
Ethically, circumcision raises concerns about consent, as it is often performed on infants or young children who cannot decide for themselves. Culturally, it may hold significant value in certain religions and communities. Ultimately, the decision to circumcise is a personal one and should be made after considering the potential health benefits, risks, and cultural or ethical beliefs surrounding the practice.

Female circumcision, also known as female genital mutilation, is a deeply controversial practice that involves the removal of part or all of the external female genitalia. Unlike male circumcision, which is associated with certain health benefits, female circumcision is recognized as a harmful practice by the World Health Organization (WHO) and other international bodies.
Female genital mutilation can lead to severe complications, including chronic pain, infertility, complications during childbirth, and psychological trauma. It is illegal in many countries, and efforts to eliminate the practice are ongoing worldwide. The procedure has no health benefits and is often performed due to cultural, religious, or societal pressure.
There are four primary types of female circumcision:

Making an informed decision as a parent, especially regarding a procedure like circumcision, requires careful consideration of various factors, including medical, ethical, cultural, and personal beliefs. It is essential to research the potential health benefits, such as reduced risks of infections and certain diseases, as well as the possible risks and complications, including pain, infection, and psychological effects. Equally important is understanding the cultural or religious significance of circumcision in your community and how that aligns with your family’s values.
Moreover, parents must consider the ethical aspect of bodily autonomy, as circumcision is often performed on infants who cannot give consent. Consulting with healthcare professionals and discussing the decision with family members can help ensure that the choice made is well-informed and in the best interest of the child’s health and future well-being.
Ultimately, the decision should be made thoughtfully, weighing both the potential benefits and risks while respecting your child’s rights and your family’s beliefs.
Circumcision is a complex and deeply personal decision for parents. Whether you are considering circumcision surgery for your son or looking to understand the potential benefits and risks of the procedure, it is essential to educate yourself on the subject. By understanding the circumcision procedure, its potential benefits, and its disadvantages, you can make an informed decision that aligns with your values and prioritizes the health and well-being of your child.
It is also important to recognise that the practice of female circumcision (FGM) is harmful and should be avoided at all costs. Education and awareness are key to eliminating this harmful practice globally.
All in all, whether circumcision is good or bad depends on your unique circumstances, and no single answer fits every situation. Make sure to consult with trusted healthcare professionals to guide your decision, keeping in mind both the health and emotional implications for your child.
Men get circumcised for cultural, religious, or medical reasons, such as improved hygiene and reduced risk of infections.
Whether circumcision is good depends on personal, cultural, or medical factors, as it offers health benefits but also carries potential risks.
Circumcision is typically performed under anaesthesia, minimizing pain during the procedure, but mild discomfort or soreness may be experienced during recovery.
Sources:
Spread the love, follow us on our social media channels